How Physical Therapy Can Help with Stress: More Than Just Injury Recovery
April 8, 2025

When you think of physical therapy, stress relief might not be the first thing that comes to mind. Most people associate it with recovering from injuries, post-surgery rehabilitation, or improving mobility. But here’s something many overlook: physical therapy can be a powerful tool in managing and reducing stress. Yes, you read that right — your physical therapist might just become your next stress-relief partner.
Let’s explore how physical therapy can help ease the tension in both your muscles and your mind.
1. The Physical-Stress Connection
Stress isn’t just in your head — it takes a toll on your body too. Chronic stress can cause muscle tension, headaches, fatigue, and poor posture. Over time, this leads to physical pain and discomfort, which only adds more stress. It’s a vicious cycle. Physical therapy steps in to break that cycle by addressing the physical manifestations of stress directly.
2. Improving Movement = Easing Mental Strain
Tension and stiffness can limit your range of motion and make everyday tasks more difficult. Physical therapists use targeted stretches, exercises, and hands-on techniques to release tight muscles and improve your mobility. As your body moves more freely, you naturally feel lighter — mentally and emotionally. Movement has a way of boosting mood and resetting the mind.
3. Breathing and Relaxation Techniques
A lot of physical therapists incorporate breathing exercises into treatment sessions. Deep, diaphragmatic breathing isn’t just good for oxygen flow — it activates the parasympathetic nervous system (a.k.a. your body’s “calm down” mode). Learning to breathe properly can lower blood pressure, reduce anxiety, and even improve sleep — all of which help manage stress.
4. Posture Correction and Body Awareness
Stress often shows up in our posture. Think rounded shoulders, clenched jaws, or a constantly stiff neck. Physical therapists help you become more aware of these physical habits and teach you how to correct them. Better posture not only helps with physical pain, but it can also improve your confidence and mindset.
5. Exercise = Endorphins
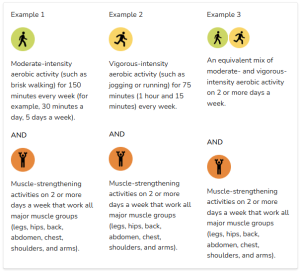
Exercise is a proven stress-buster. Physical therapists can design customized exercise plans that are safe, effective, and tailored to your lifestyle. Whether it’s light stretching, strength training, or gentle cardio, regular physical activity releases endorphins — your body’s natural feel-good chemicals. Plus, having a guided routine can give you structure and a sense of accomplishment.
6. A Supportive, Healing Environment
Sometimes, just having someone listen and guide you can relieve stress. Physical therapy often involves one-on-one attention, where your concerns are heard and your progress is celebrated. That sense of care and support can be incredibly grounding during high-stress times.
Stress is a whole-body experience — and it deserves a whole-body approach. Physical therapy isn’t just about healing injuries; it’s about restoring balance in your body and mind. Whether you’re dealing with chronic stress or just feeling a little off, incorporating physical therapy into your wellness routine might be the reset you didn’t know you needed.
So, the next time stress weighs you down, consider stepping into a physical therapy clinic. Your mind — and your muscles — will thank you.